BACKGROUND
Lymphoblastic lymphoma, a rare non-Hodgkin's lymphoma subtype, exhibits striking cytological and histological parallels with acute lymphoblastic leukemia (ALL). Such similarities have led to its classification as precursor B and T lymphoblastic lymphoma/leukemia by the World Health Organization. Exhibiting a modest global incidence of 1 to 5 cases per 100,000 population, it is notable that two-thirds of cases of ALL cases are of B-cell phenotype (PMID 15698386). To deepen our comprehension of this rare disease, it becomes essential to understand its behavior across various demographics, particularly among Hispanic (HI) and Non-Hispanic (NH) populations in the United States (US). To bridge this knowledge gap, this pioneering nationwide study endeavors to unravel how demographic, clinical, and survival outcomes vary between HI and NH patients with this disease.
METHODS:
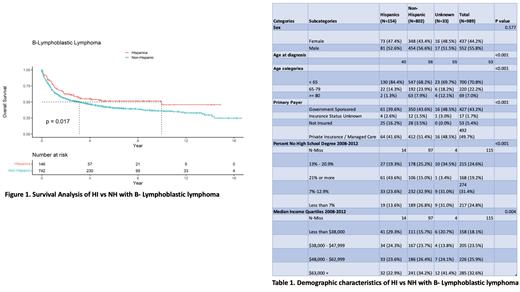
Data were analyzed on B-Lymphoblastic lymphoma patients in the US reported to the National Cancer Database (NCDB) between 2004 and 2019. Demographic and treatment characteristics were compared between ethnic groups. Kaplan-Meier and Cox regression analyses were used to compare OS between Hispanic and Non-Hispanic populations. Multivariate analysis and propensity score matching was performed with adjustment for age, stage, co-morbidity score, and insurance status, type of facility and great circle distance.
RESULTS
Of 989 B-Lymphoblastic Lymphoma patients, 16 were HI, and 81% NH. 53% of HI were male, compared to 57% of NH.
At diagnosis, HI patients were younger (40 years vs. 56 years) (p=<0.001); the majority of HI 84% and NH 68% were diagnosed in the age bracket of < 65 (p=<0.001).
With respect to race, most of both HI and NH were whites (87% vs 85%), followed by blacks (1% vs 10%). Examining the stage, most of both HI 45% and NH 47% were stage IV (p= 0.260).
When looking at insurance type; private insurance was the most prevalent type in HI vs NH (42% vs 51%), followed by government-sponsored (40% vs 44%). The most uninsured group was HI 16% vs NH 3%.
Considering Census Median Income (2008-2012), the most prevalent bracket for HI was Less than $38,000 (29%) and NH was $63,000+ (34%). When it comes to median income of less than $38,000, HI were 29% vs NH 16%.
As for Charlson-Deyo Score (comorbidities score), HI had 10% =/> 2 scores, vs NH 8%. In terms of Academic/Research Programs, including NCI-designated comprehensive cancer centers, it was the most prevalent type of facility providing care for both HI 55% and NH 50%.
Regarding the median distance in miles between the patient's residence and the hospital that reported the case (Great Circle Distance), HI lived at a median of 9.3 miles, vs NH at a median of 12.4 miles.
On survival analysis; the survival probability at 2, 5, and 10 years of HI vs NH were (0.624 vs 0.552), (0.516 vs 0.435), and (0.458 vs 0.362), respectively. The median survival time (MS) was 10.0 years for HI, vs 3.1 years for NH; and there was an overall survival (OS) difference favoring HI with (p=0.017).
On multivariate analysis, there were no independent variables associated with better or worse OS; however, the propensity matched analysis showed a striking MS difference between HI vs NH (3.02 y vs. 1.43 y).
CONCLUSION
This groundbreaking study provides crucial insights into the distinct demographic and clinical characteristics of HI and NH patients with B-Lymphoblastic Lymphoma in the US. Importantly, we found that HI patients were significantly younger at diagnosis, and despite having a higher percentage of uninsured individuals and lower median income, showed better survival outcomes compared to NH. These findings highlight the critical role ethnicity plays in disease presentation and prognosis, thus emphasizing the importance of culturally sensitive, tailored healthcare approaches. This study underscores the urgent need for further research to understand intrinsic biologic factors contributing to these disparities and enhance health equity in lymphoma care.
Disclosures
Diaz Duque:Morphosys: Consultancy; Lilly: Consultancy; ADCT: Consultancy; AstraZeneca, ADCT, Lilly, Morphosys, Genentech: Consultancy, Honoraria; Genentech: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal